Table of Contents
How to Build an AI-Powered Mental Health App | Features, Cost & Compliance Guide
Author

Subject Matter Expert

Date

Book a call
When therapy waitlists stretch for months, AI can step in within seconds. Mental health issues are no longer a silent epidemic—they are a daily reality for millions. Yet, access to timely, personalised care remains a significant gap, especially in the U.S. That’s where AI-powered mental health apps are rewriting the rules, offering scalable, 24/7 support through intelligent chatbots, mood tracking, and behavioural coaching.
For businesses and digital health innovators, this is not just a solution—it’s an opportunity. With the U.S. market for mental wellness apps surging, investing in AI-driven tools is both timely and strategic.
In this blog, we will explore the rising demand, app types, development roadmap, essential features, costs, challenges, and how we help build future-ready solutions.

The Growing Demand for AI-Powered Mental Health Apps
Rising stress levels, loneliness, and clinical anxiety are pushing millions to seek support, but traditional care systems are overwhelmed. In the U.S. alone, over 50 million adults face mental health issues annually, with many unable to access timely help. AI-powered mental health apps bridge this gap with 24/7 availability, intelligent mood tracking, and scalable cognitive support.
Globally, the mental health app market was valued at $5.2 billion in 2022 and is expected to grow at a 15.9% CAGR through 2030. AI mental health apps use NLP, machine learning, and emotion recognition to deliver therapy-like experiences. Common types include CBT-based apps, journaling tools, guided meditation platforms, and AI chatbots, making care more personalized, private, and proactive.

At the Healthcare Meetup 2025 hosted by GeekyAnts at Microsoft Reactor, Apoorva Sahu, Director of Product Engineering at GeekyAnts, explores how AI is reshaping mental healthcare. He highlights cutting-edge tools like facial expression analysis and emotional tracking that are driving ethical, scalable, and accessible solutions.
Types of Mental Health Applications: Real Use, Real Impact
Mental health tech is not evolving—it’s surging. With over 20 million users relying on mental wellness apps in the U.S. alone and global downloads surpassing 300 million, AI is quietly becoming the invisible therapist. Each app type below serves a distinct, high-impact function in how care is accessed and delivered.
1. Self-Monitoring & Mood Tracking Apps
Platforms like MindDoc, with over 2.5 million users, turn routine mood check-ins into early warning systems. By analyzing emotional trends, sleep cycles, and behavioral patterns, these apps help surface issues before they become clinical. The AI doesn’t wait for you to ask—it detects the shift.
Why it matters: Prevents silent mental health declines
Core Role: Proactive emotional insight engine
Use Case: Burnout detection, pre-therapy self-awareness
2. Cognitive Behavioral Therapy (CBT) Apps
Used by more than 5 million users globally, apps like Woebot deliver evidence-based CBT techniques through real-time conversations. Instead of static modules, users interact with AI that adapts based on emotional tone and phrasing, reconstructing negative thought patterns through structured, human-like guidance.
Why it matters: Democratizes CBT, 24/7
Core Role: Digital therapist assistant
Use Case: Anxiety regulation, cognitive reframing
3. AI-Powered Chatbots
Wysa, downloaded over 10 million times, acts as a front-line responder when licensed professionals aren’t available. The chatbot applies NLP and GenAI to hold therapeutic-grade conversations, offering coping strategies and even triggering escalation when emotional red flags are detected.
Why it matters: Fills the human gap with safety and scale
Core Role: On-demand emotional triage
Use Case: Night-time anxiety, stress spirals, therapy waitlist support
4. Meditation & Mindfulness Apps
With Headspace serving over 70 million users, AI now personalizes calm. The app tailors meditation flows, audio content, and reminders based on behavioral insights, pushing shorter, high-impact sessions during workdays and longer ones during recovery phases.
Why it matters: Mindfulness that adapts to mental state
Core Role: Dynamic mental fitness trainer
Use Case: Stress reduction, daily mental reset, sleep therapy
5. Online Therapy Platforms
Platforms like Talkspace, trusted by over 1 million users, reduce therapy onboarding friction. AI-driven intake forms match patients with therapists based on cognitive and emotional profiles, not availability, while some platforms use AI to track post-session sentiment and engagement.
Why it matters: Shortens access time, improves fit
Core Role: Precision therapy delivery system
Use Case: Matched counseling, long-term care optimization
6. Crisis Support Apps
The notOK App, featured by NAMI and growing among Gen Z users, offers a one-touch emergency alert system. More critically, its AI learns user behavior to predict escalation before the SOS is triggered—an evolving safety net for high-risk moments.
Why it matters: Moves from reactive to predictive crisis care
Core Role: AI-powered escalation layer
Use Case: Suicide prevention, relapse alerts, high-risk monitoring

Step-by-Step Guide to Developing an AI-Powered Mental Health App
This guide isn’t built on theory—it’s built on what we’ve delivered. At GeekyAnts, we have helped build AI-driven mental health solutions that are not only functional and scalable but also safe, compliant, and deeply human-centred. What follows is a step-by-step roadmap based on that experience, designed to help product teams and founders bring meaningful mental wellness apps to lif

1. Define the Core Mental Health Use Case
Every successful mental health app begins with a focused problem. General wellness won’t resonate in a saturated market, but a product that addresses burnout in working professionals or provides CBT support for anxiety stands out.
This early decision shapes everything: your tech stack, AI model, user flows, and compliance needs.
Real-world lesson: In one of our projects, narrowing the use case to postpartum emotional health resulted in higher user engagement and more targeted interventions.
2. Conduct Market Research and Compliance Planning in Parallel
It’s essential to know what’s working and what isn’t. Study apps like Wysa, Calm, and BetterHelp. Look at app store reviews, user forums, and product update logs. Identify pain points you can solve better.
At the same time, understand what regulations apply. If your app handles any form of health data in the U.S., HIPAA applies. Waiting to address compliance until after development is a costly mistake.
Start validation and regulation planning side by side. They are not separate tracks—they move together.
3. Prioritize UX for Emotional Safety
Users won’t always arrive at your app in a stable emotional state. The design must reflect this. Avoid harsh colors, complex flows, or technical language. Every interaction should feel intentional, calming, and easy to navigate.
Best practice: Enable anonymous entry points. Let users explore the app before creating an account or sharing personal details. This increases adoption and builds early trust.
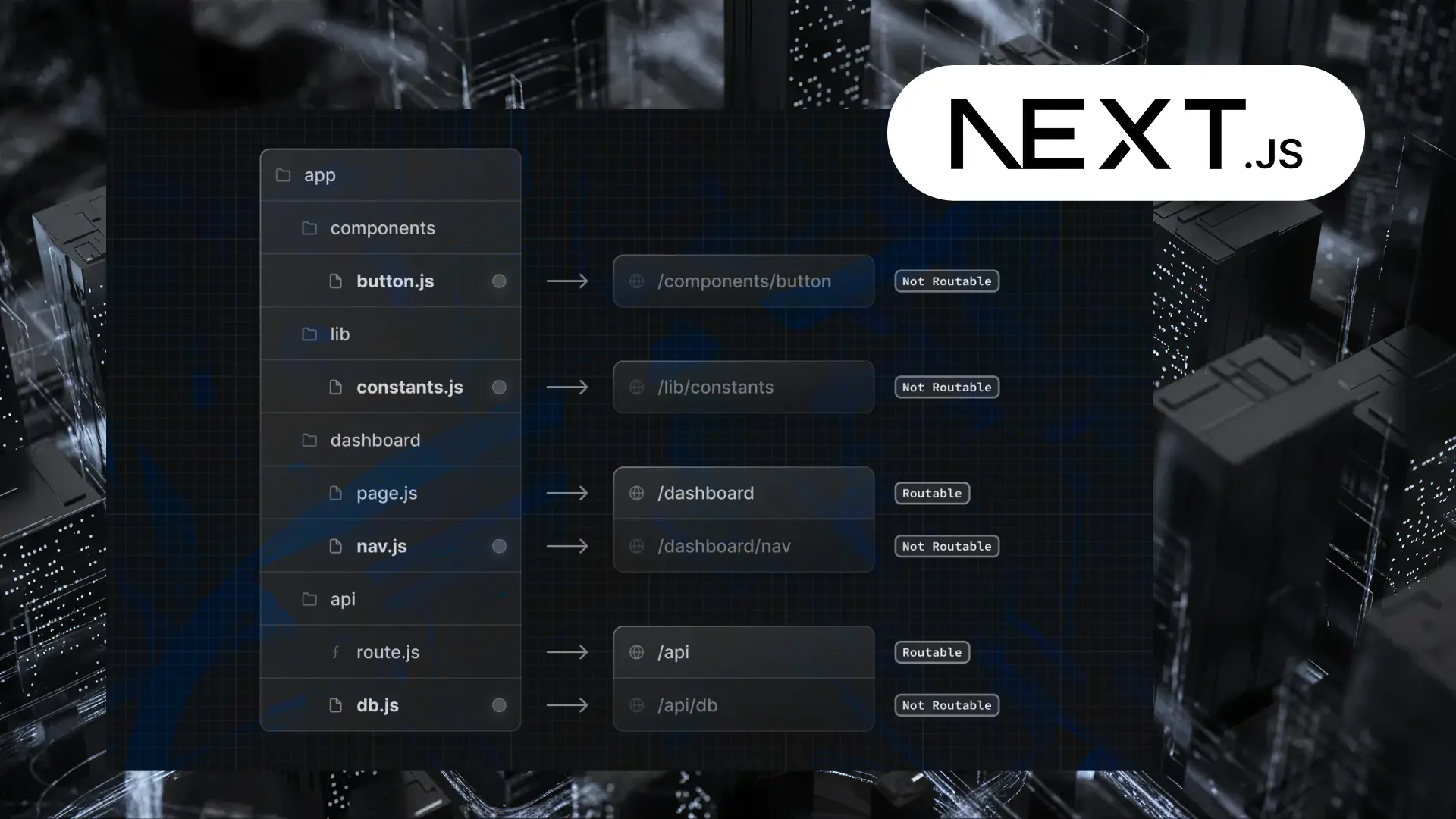
4. Choose a Scalable Tech Stack and the Right AI Tools
The backbone of your app needs to be lightweight, scalable, and secure. At GeekyAnts, we often use React Native for cross-platform development, backed by Node.js or Django for robust server-side logic.
For AI, you’ll need:
- NLP engines like Dialogflow, GPT-4, or BERT for chat experiences
- Sentiment detection models to track mood patterns
- Recommendation systems to deliver personalized activities and content
What you choose should align with the problem you're solving, not just with what's trending.
5. Build the MVP with a Clear Purpose
Your minimum viable product is not a feature buffet—it’s a focused solution. Begin with:
- An AI-powered chatbot
- Mood journaling with analytics
- Reminders or emotional check-ins
- A secure, HIPAA-compliant user profile
The goal is to solve one key problem exceptionally well. Add sophistication only after you validate the foundation.
6. Integrate AI Responsibly and Thoughtfully
AI in mental health is not a shortcut. It must be trained carefully, using validated psychological frameworks like CBT or ACT. Your AI model should recognize when it’s out of its depth and escalate to a human support system.
Set clear limitations. Define fallback logic. Avoid storing personal health information unless you need it—and if you do, ensure it’s encrypted and access-controlled.
Industry case: A UK-based mental health app faced public scrutiny after its AI chatbot failed to detect crisis language, proving that ethical safeguards are non-negotiable.
7. Test with Real Users and Clinical Advisors
Testing isn't about finding bugs—it's about finding out whether your app supports people meaningfully. You’ll need feedback from both ends:
- The people using your app during stressful or anxious moments
- The professionals who understand therapeutic models and ethical boundaries
Refine onboarding flows. Observe emotional responses to bot conversations. Use this phase to validate your assumptions and identify gaps before scaling.
8. Launch Gradually with Smart Monitoring
Don’t launch everything at once. Start small. Use analytics tools to observe:
- Retention behavior
- Drop-offs during chat interactions
- Peak usage times
- Sentiment trends over time
Your first few hundred users will shape the future of your roadmap—if you listen closely.
9. Maintain Ongoing Compliance and Continuously Improve Your AI
Your AI model won’t stay relevant unless it learns. Regular retraining on anonymized data (with user consent) is key. Keep audit logs for AI decisions, especially in therapeutic scenarios.
Likewise, compliance is an ongoing process. HIPAA, GDPR, and local regulations evolve. Schedule regular audits, update policies, and review your data pipelines often.
Manual override mechanisms are essential. Every AI-driven experience must include a human fail-safe.
10. Plan for Longevity: Monetization and Scalability
From the start, think about how your app will sustain itself. Common models include:
- Freemium with in-app upgrades
- Subscription tiers
- B2B partnerships with employers or schools
- Licensing to clinics or wellness platforms
Each model affects how you build. BetterHelp, for instance, scaled by combining user subscriptions with enterprise partnerships.
This step-by-step process reflects our real-world experience in building AI-powered mental health apps that are technically sound, ethically grounded, and built for long-term impact. Whether you’re launching a targeted MVP or preparing for national scale, this roadmap will help you avoid common pitfalls and build with clarity from day one.
Mental Health App Development Best Practices
Developing a mental health app is not a design sprint. It is a responsibility. You are not building a feature—you are building a fallback system for people who may have no one else at that moment. I have worked with therapists in whiteboard sessions, handled releases in crises, and fixed user feedback while they faced panic, trauma, and recovery. These are the practices that have proven non-negotiable.
1. Start with clinicians in the room
During our first mental health project, we made the mistake of designing journaling prompts ourselves. A licensed psychologist reviewed them and flagged three as potentially triggering. That was the last time we wrote without clinical input. Since then, every major feature—whether CBT modules or intake flows—have been co-developed with therapists.
Best Practice: Bring licensed professionals in from day one. Let them shape the core, not review it after.
Avoid: Guessing user needs based on blog research. Clinical alignment is not optional.
2. Design for mental clarity, not user retention
In one usability test, a user froze during onboarding. The avatar was cheerful, the color palette bright, but the language felt invasive. That moment changed our UX strategy. From then on, we prioritized psychological safety: soft visuals, opt-out flows, zero-judgment microcopy.
Best Practice: Design for comfort. Allow anonymity. Give space. Let users disengage without penalty.
Avoid: Forced personalization or guilt-based notifications. Respect disengagement.
3. Handle data like it belongs to a patient, not a product
Every app collects data. Mental health apps collect vulnerability. I have seen teams overlook encryption layers because “it was only a mood tracker.” That is a critical mistake. Mood logs, journal entries, session notes—these are medical-grade artifacts. Your infrastructure must reflect that.
Best Practice: Apply HIPAA and GDPR as defaults. Encrypt everything. Use role-based access.
Avoid: Storing data in shared environments or deferring compliance until scale.
4. Use AI as an assistant, not a therapist
We built an AI triage bot that could detect signs of emotional distress using sentiment scoring. It worked—until we pushed it too far. The model began suggesting advice instead of deferring to a human. That was the point we defined the line: AI supports, never substitutes. All outputs must allow escalation and override.
Best Practice: Train AI on validated frameworks. Insert human fallback. Monitor all decision logic.
Avoid: Letting models simulate empathy or give clinical suggestions without constraints.
5. Test in context, not in conference rooms
In early beta testing, one participant exited the app during a panic journaling session. The reason? The “Back” button vanished mid-input. That taught us something most usability tests miss: emotional context changes how users interact. You are not testing an app. You are testing how someone will use it during fear, grief, or disconnection.
Best Practice: Conduct trauma-informed testing. Observe usage during stress-simulated sessions.
Avoid: Standard QA loops. Controlled environments do not reflect reality.
6. Build for change, not completion
User needs shift. Regulations evolve. In one release cycle, we had to refactor an entire intake process after new state-level privacy laws. It was painful because we had hardcoded everything. Now, we modularize features, run clinical audits, and embed in-app feedback loops.
Best Practice: Schedule model retraining. Version features like clinical protocols. Plan for iteration.
Avoid: Locking workflows or models. Flexibility is part of responsibility.
Key Features of an AI-Powered Mental Health App
Effective mental health apps combine clinical intelligence, AI-driven personalization, and secure design. Here are the essential features that matter:
1. AI Chatbot Support
NLP-powered conversations modeled on CBT/DBT frameworks for real-time, guided emotional support.
2. Mood & Sentiment Tracking
Journaling with AI analysis to detect patterns and deliver behavior-based nudges.
3. Personalized Content Engine
Adaptive recommendations for exercises, routines, and self-care prompts based on user input.
4. Crisis Escalation Logic
Immediate routing to emergency contacts or helplines during high-risk moments.
5. HIPAA-Compliant Security
End-to-end encryption, anonymized modes, and strict data controls.
6. Progress Dashboard
Visual insights into emotional trends, completed goals, and self-reflection history.
Cost of Developing a Mental Health App with AI Integration
The cost of building an AI-powered mental health app depends on features, AI complexity, compliance requirements, and team expertise. Here's a clear breakdown:
| App Tier | Features Included | Estimated Cost (USD) | Development Time |
| Basic App | - Mood tracking - Basic journaling - Simple chatbot with rule-based replies - Basic UI/UX | $40,000 – $60,000 | 3 – 4 months |
| Mid-Level App | - NLP-based chatbot - Sentiment analysis - Personalized content engine - HIPAA compliance - User analytics dashboard | $70,000 – $120,000 | 5 – 7 months |
| Advanced App | - AI-powered CBT therapy bot - Real-time emotion detection - Crisis escalation system - Wearable integration - Therapist portal - Voice journaling - End-to-end security | $130,000 – $200,000+ | 8 – 10+ months |
Note: Costs may vary based on team location, tech stack, and whether features like multilingual support, third-party integrations, or AI training pipelines are included.
Challenges and Ethical Considerations
In AI-driven mental health apps, every technical decision carries ethical weight. These platforms are not entertainment products; they interact with users during moments of stress, uncertainty, and sometimes crisis. Precision alone is not enough—engineers must incorporate care into the system.
1. Data Sensitivity and User Privacy
Mental health data is deeply personal. Users often hesitate to engage when onboarding demands excessive information upfront.
Solution: Privacy-first systems must be prioritized, supporting anonymous journaling, encrypted sessions, and minimal data retention by default. Compliance with HIPAA and GDPR should be integrated into the architecture rather than added post-launch.
2. Bias in AI Training and Response
AI models trained on narrow or unbalanced datasets can misinterpret tone and emotion, resulting in inconsistent or inappropriate responses across user segments.
Solution: AI should be trained on clinically vetted, demographically diverse datasets. Therapist-guided reviews help ensure consistent tone and response quality across scenarios. Bias testing must meet strict thresholds before any deployment.
3. Over-Reliance on Chatbots in High-Risk Moments
In high-risk cases, AI chatbots may default to general tips rather than identifying and escalating serious emotional signals.
Solution: Real-time escalation logic is essential. Sentiment analysis and keyword triggers should route high-risk conversations to clinical support or emergency helplines. Systems must be built to recognize their limitations and defer accordingly.
4. Lack of Explainability in AI Decisions
Unexplained AI behavior undermines user trust, especially in contexts involving emotional guidance or therapeutic recommendations.
Solution: Every AI decision flow should include audit trails and transparent logic. Therapists must have access to review, trace, and override outputs where necessary. Black-box models are unsuitable for live deployment in mental health environments.
5. Delayed or Reactive Compliance Strategy
Retrofitting compliance into an existing app architecture can lead to costly delays and risk exposure.
Solution: Compliance must be foundational. Modular frameworks should be designed to support HIPAA, GDPR, and regional data laws from the outset. Legal audits should be scheduled throughout the product lifecycle.
6. Poor Emotional UX Design
Interfaces that work for general-purpose apps can alienate or overwhelm users in mental health contexts. Cluttered layouts or vibrant visuals may trigger disengagement.
Solution: Emotionally sensitive design principles should guide every interface decision. Minimalist layouts, calming color palettes, and optional input flows help reduce cognitive load. UX flows must be validated by mental health professionals.
Exploring the Role of AI in the Future of Mental Health App and Support
AI continues to expand the boundaries of digital mental health care, moving from reactive tools to intelligent, proactive support systems. Current apps use AI for real-time emotional guidance, mood tracking, and behavior-based recommendations. The future lies in emotionally aware systems capable of interpreting tone, language, and biometric cues to detect psychological shifts early. Integration with wearables like Apple Watch or Fitbit will enable continuous monitoring, prompting timely interventions.
Emerging LLMs will support therapy continuity by retaining context across sessions, enhancing personalization without sacrificing privacy. Some platforms are advancing toward multi-modal AI that combines voice, text, and passive data for deeper insight. At GeekyAnts, we’re already building solutions that merge adaptive UX with HIPAA-aligned architecture and AI-driven personalization. The next generation of mental health apps will deliver care that feels human, contextual, and clinically reliable—at scale.
How GeekyAnts Can Help You Develop a Custom AI-Powered Mental Health App
GeekyAnts has worked extensively on building mental health applications with a focus on AI integration, data security, and clinical usability. Our collaboration on MariGold Health involved developing features such as emotion-based journaling, secure messaging, and real-time engagement workflows, while ensuring HIPAA compliance throughout the architecture.
We specialize in building modular, scalable systems that incorporate NLP, sentiment analysis, and therapist support layers. Our teams follow a structured process—from understanding regulatory requirements to designing UX flows suitable for emotionally sensitive users. Whether the requirement is a simple AI chatbot or a hybrid therapy model with professional oversight, we develop systems grounded in real-world healthcare logic and technical precision.
Conclusion
Developing an AI-powered mental health app demands more than technical proficiency—it requires a deep understanding of clinical ethics, user behavior, and scalable system design. From selecting the right AI models to ensuring HIPAA compliance and emotional UX, every step must be deliberate and user-first. As mental health challenges grow in complexity, so must the solutions. AI offers the ability to deliver personalized, proactive care—but only when implemented with care, context, and oversight. This guide reflects what we have learned through hands-on experience: that building for mental wellness means building with responsibility. For teams ready to take that step, the opportunity is both urgent and meaningful.
FAQs
1. How can mental wellness apps integrate with existing healthcare systems?
Integration happens through APIs and secure data protocols. You can sync with EMRs (Electronic Medical Records), telehealth platforms, or insurance systems using HL7 or FHIR standards, while ensuring HIPAA compliance. This enables smooth data sharing between patients, apps, and care providers.
2. Can AI completely replace human therapists?
No. AI can augment therapy with 24/7 support, mood tracking, and self-help tools, but it cannot replace human empathy or clinical judgment. The most effective apps use a hybrid model—AI for day-to-day support and therapists for complex needs.
3. Which tech stacks should I consider to develop a mental health app that relies on AI?
- Frontend: React Native or Flutter
- Backend: Node.js, Django, or Firebase
- AI Tools: Dialogflow, GPT APIs, TensorFlow
- Compliance: AWS/GCP with HIPAA-grade infrastructure
Choose based on scalability, team skillsets, and compliance requirements.
4. How long does it take to build an average mental health tracker app?
It typically takes 3–4 months for a basic version, and 6–10+ months for a full-featured app with AI, compliance, and therapist modules. Development timeline depends on features, tech stack, and team size.
5. Does my mental fitness app need to be HIPAA compliant?
Yes, if your app collects, stores, or transmits health-related data for U.S. users. Even basic journaling apps should plan for HIPAA early to avoid costly rebuilds later.
6. Are mental health apps confidential and secure?
They can be—if built with the right security layers:
- End-to-end encryption
- Secure login (e.g., biometrics, 2FA)
- Role-based access control
- Anonymous user modes
Security is not optional; it’s foundational to user trust.
7. What’s the best monetization model for a mental health app?
That depends on your audience and goal. Popular models include:
- Freemium: Basic features are free, and advanced tools are paid
- Subscriptions: Monthly or yearly plans
- B2B Licensing: Sell access to clinics, schools, or employers
- In-app purchases: One-time feature upgrades or content packs
Choose a model that aligns with both accessibility and long-term sustainability.